Prostate Cancer by the Numbers: The Shocking Stats No One Talks About
Discover shocking prostate cancer statistics — from diagnosis rates to survival trends and screening gaps. Learn why 1 in 8 men are affected and why awareness matters more than ever in 2025.
Chris Willard
9/16/20258 min read
“1 in 8 men will be diagnosed with prostate cancer.” The first time I read that stat, I froze. That’s not some rare, one-in-a-million scenario that’s your dad, your brother, your best friend from work. And yet, we don’t talk about it nearly enough.
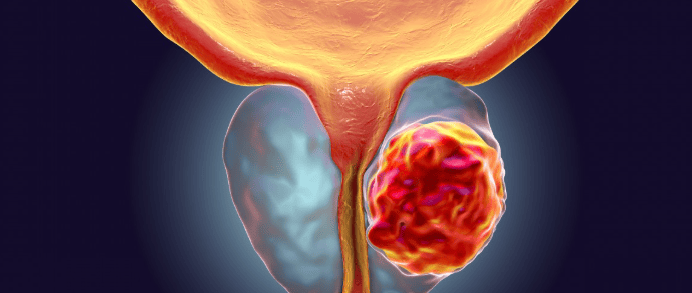
Prostate cancer is the second most common cancer in men worldwide, and while survival rates are often high with early detection, the silence around it is deafening. Too many men avoid screenings. Too many families get blindsided because nobody had “the talk” about risk factors.
In this post, I’m breaking it all down incidence, survival, screening gaps, risk factors, and why advocacy matters more than ever. Think of it like a reality check in plain English, with some snackable numbers you can take straight to your next family dinner or even share on social. Because the truth is: prostate cancer isn’t just a men’s health issue. It’s a family issue.
Incidence and Diagnosis Rates
Let’s start with the sheer scale of this disease. Prostate cancer isn’t rare it’s one of the most common cancers in men. Globally, more than 1.4 million men are diagnosed every single year, making it the second most frequently diagnosed cancer in men worldwide. In the U.S. alone, the American Cancer Society estimates about 288,000 new cases annually. That’s like filling up an NFL stadium with newly diagnosed men every year.
And here’s the stat that always makes people pause: 1 in 8 men in the U.S. will be diagnosed with prostate cancer during their lifetime. Picture a family barbecue, a group of coworkers, or even a fantasy football league odds are, at least one person in that group will face this diagnosis. When I first learned that it turned an abstract number into something personal.
But the story doesn’t stop there. Prostate cancer risk isn’t evenly distributed. Age is a major factor: the average age at diagnosis is 66, and the risk skyrockets after 50. I’ve sat in support groups where nearly every man said the same thing: “I thought I was too young to worry about it.” The truth? Even men in their early 40s can be diagnosed, especially if they have family history or genetic risk factors.
Ethnicity adds another layer. African American men face about a 70% higher incidence rate compared to white men and they’re also more likely to be diagnosed at advanced stages. On top of that, they have more than double the risk of dying from the disease. These disparities aren’t just medical; they reflect deeper issues of access to care, socioeconomic factors, and systemic gaps in health education.
So why do the numbers keep shifting? A big piece of the puzzle is screening. In the past decade, PSA (prostate-specific antigen) testing guidelines have changed more than once. Some organizations scaled back on recommending routine screenings, worried about overdiagnosis and unnecessary treatments. While well-intentioned, this decision also led to fewer men being screened early and more cancers being discovered at later, more dangerous stages.
The takeaway? Prostate cancer is common, often silent in its early stages, and unevenly distributed across age and ethnicity. The way we diagnose it is shifting, but one thing hasn’t changed: the earlier it’s caught, the better the outcomes. Numbers like these aren’t just statistics they’re reminders to keep this conversation alive.
Survival Rates and Prognosis
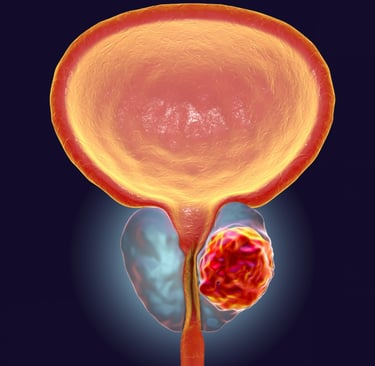
When people first hear the words “prostate cancer,” fear usually takes over. But here’s the hopeful reality: if it’s caught early, the odds of survival are overwhelmingly in your favor. For men diagnosed with localized or regional prostate cancer, the 5-year survival rate is nearly 100%. In fact, many men live well beyond 10 years post-diagnosis without the cancer ever returning. That’s one of the strongest survival stories in oncology.
The picture changes, though, when cancer spreads beyond the prostate. Once it reaches distant parts of the body — bones, lymph nodes, or other organs the 5-year survival rate drops to about 32%. That’s a massive gap, and it underscores why early detection isn’t just important, it’s lifesaving. I once met a survivor who said, “I got lucky. Mine was caught by accident on a routine test.” His story stuck with me because without that early catch, his outcome could’ve looked very different.
Advances in treatment have also shifted the survival landscape. Robotic-assisted surgeries now mean less recovery time and fewer complications. Radiation therapies have become more precise, targeting tumors without damaging as much surrounding tissue. And newer treatments like immunotherapy and targeted hormone therapies are helping men with advanced cases live longer, fuller lives. What was once considered a near-certain death sentence 20 years ago is now, for many, a manageable chronic condition.
But here’s something a lot of people don’t realize, prognosis isn’t a one-size-fits-all prediction. It’s deeply personal. A man’s survival odds depend not just on the stage of his cancer, but on his age, overall health, family history, and even genetic markers. Doctors are getting better at tailoring treatment plans based on those factors, which means outcomes are more individualized than ever.
Early detection remains the single most powerful predictor of survival. A prostate cancer caught at stage I or II has a vastly different trajectory than one discovered at stage IV. That’s why conversations about PSA testing, digital rectal exams, and family history aren’t just awkward doctor visits — they’re potential life-saving steps.
So, if there’s one thing the survival statistics teach us, it’s this: the earlier you know, the better your chances. Numbers don’t lie, and in this case, they’re practically shouting at us to pay attention.
Screening Gaps and Challenges
Screening is where the whole story of prostate cancer can change but it’s also where too many men slip through the cracks. The PSA (prostate-specific antigen) test is one of the simplest tools we have, yet only about 60% of men over 50 report getting screened regularly. That means almost half of the men who should be having these conversations aren’t.
Why the hesitation? Honestly, I’ve heard it all. Some men think, “I don’t have symptoms, so why bother?” Others avoid it because of the stigma let’s be real, talking about your prostate doesn’t exactly come up at the dinner table. And then there’s the confusion created by changing guidelines. A few years ago, major health organizations pulled back on recommending routine PSA testing, worried it was leading to too many unnecessary biopsies and treatments. While their intentions were good, the unintended fallout was fewer men being screened and more cancers being caught at later, more dangerous stages.
Access to care is another major barrier. If you live in a rural community or don’t have health insurance, just getting to a urologist can feel like climbing a mountain. I’ve spoken to men who put it off for years simply because they didn’t want to deal with the hassle or the cost. That delay can mean the difference between a curable cancer and one that’s already spread.
The problem isn’t evenly spread either. African American men, who already face higher risk and worse outcomes, are less likely to be screened early and regularly. Men in lower-income communities or without a primary care doctor are also underserved. Even within the “recommended” age groups, there’s a gap, men in their early 50s sometimes assume they’re too young, and older men assume it’s too late to matter. Both assumptions are dangerous.
When I asked a friend why he skipped his PSA test, he shrugged and said, “I feel fine.” That’s the catch, prostate cancer often has no symptoms in its early stages. By the time you “feel” something is wrong, the disease may already be advanced.
So, here’s the takeaway: the PSA test isn’t perfect, but it’s still one of the best early-warning systems we have. Until we break down the barriers of stigma, misinformation, and access, the screening gap will continue to cost lives.
Prostate Cancer Risk Factors You Can’t Ignore
If there’s one thing I’ve learned from listening to survivors and doctors, it’s this: prostate cancer doesn’t happen in a vacuum. There are patterns, risk factors that stack the odds. Some you can change, some you can’t, but all of them matter.
Let’s start with the big one: family history. If your dad or brother had prostate cancer, your risk doubles. Add in certain genetic mutations like BRCA1 or BRCA2 (the same ones linked to breast cancer), and the danger climbs even higher. I once talked to a man who said, “I thought BRCA was just for women.” Nope, those genes don’t discriminate. Knowing your family history could literally save your life.
Then there’s lifestyle. Research has connected obesity, poor diet, and lack of exercise to higher prostate cancer risk. Diets heavy in processed meats and low in fruits and vegetables don’t do your prostate any favors. On the flip side, men who stick to balanced diets with more plant-based foods, omega-3s, and regular physical activity tend to fare better. I remember a survivor saying, “The hardest part wasn’t treatment it was rethinking how I ate every single day.” That shift can feel overwhelming, but it’s one risk factor you actually have some control over.
Race and socioeconomic status add another layer of complexity. African American men not only face higher risk of developing prostate cancer but also tend to get more aggressive forms of the disease. Add limited access to quality healthcare or delays in screening because of cost, and the risks multiply. This isn’t just biology; it’s also about systemic inequities that leave some men more vulnerable than others.
And let’s clear up a few myths, because they’re still floating around in conversations I’ve had. No, frequent sex doesn’t increase your risk. Cycling won’t damage your prostate in a way that causes cancer. And vasectomies? There’s no credible evidence linking them to higher prostate cancer risk. Yet I’ve heard these myths repeated so many times they almost sound believable. The truth is, focusing on evidence-based risks like family history, genetics, lifestyle, race, and access to care is where men should put their attention.
At the end of the day, risk factors aren’t meant to scare you they’re meant to empower you. You can’t change your DNA or your race, but you can know your family history, talk to your doctor early, and make choices that stack the odds in your favor.
Awareness, Advocacy, and the Road Ahead
Here’s the hard truth: prostate cancer doesn’t get the spotlight it deserves. When October rolls around, you can’t walk through a grocery store without seeing pink ribbons for breast cancer awareness. But September, which is Prostate Cancer Awareness Month, often passes quietly. That lack of visibility shows up in the numbers too: funding for prostate cancer research lags behind, even though it’s the second most common cancer in men worldwide. Awareness matters because funding follows attention, and without it, breakthroughs slow down.
Fundraising gaps are real. Prostate cancer receives significantly less per-patient research funding compared to breast cancer or even less common cancers. That leaves holes in everything from cutting-edge treatment trials to community screening programs. Policy change could help things like expanding insurance coverage for PSA testing, improving outreach to underserved communities, and prioritizing men’s health in national health agendas. But those shifts won’t happen without pressure from the ground up.
That’s where patient advocates and caregivers come in. Honestly, they’re the heartbeat of awareness. I’ve been in rooms where one survivor sharing his story changed the way ten other men thought about screening. Caregivers, too, play a huge role. They’re often the ones pushing loved ones to the doctor, organizing local support groups, or raising funds when the system falls short. Advocacy doesn’t always look like a march on Capitol Hill, sometimes it’s a caregiver reminding her husband, “Hey, you need that PSA test.”
And here’s the encouraging part: awareness is contagious. I’ve seen one social media post spark a conversation at a dinner table, which then leads a man to book a screening the next week. That’s the power of breaking the silence. The more we share stories, the more we normalize the conversation around prostate cancer, and the harder it becomes to ignore in public health conversations.
So what’s the road ahead? It’s us. Men speaking up about their diagnoses. Families sharing the tough parts of the journey. Communities fundraising, even in small ways. And all of us pushing for better screening policies and equal access to care.
If you’re reading this, you can be part of that movement. Share the statistics. Support a local awareness event. Encourage the men in your life to get screened. Because every voice added is another step toward making sure prostate cancer gets the visibility it desperately needs.
© The Advocate Voice | All Rights Reserved
